analysis of the causes of coma caused by different parts of the brain
- 2025-03-11
- Dr. Xiao
- 157
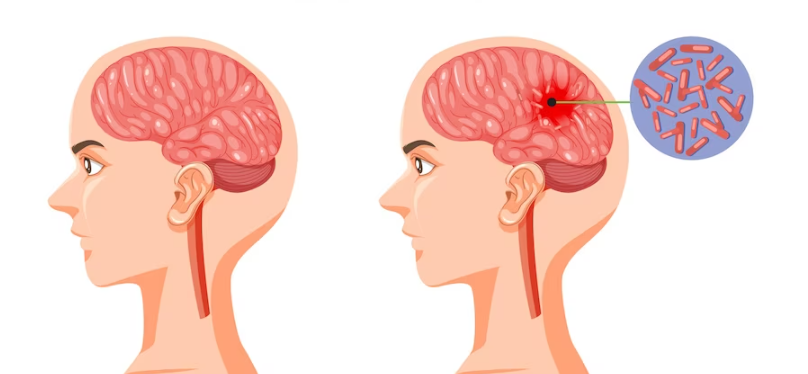
analysis of the causes of coma caused by different parts of the brain. today i will introduce to you,what are the conditions of supratentorial space-occupying lesions?
supratentorial space-occupying lesions mainly include the cerebral hemispheres, the cerebral cortex, corticolimbic reticular activating system, thalamic non-specific projection system, central part of the diencephalon and the ascending reticular activating system of the midbrain related to coma. damage can lead to coma. only damage to the ascending reticular activating system in the central part of the diencephalon or midbrain on one cerebral hemisphere can cause coma. unilateral cerebral hemisphere occupation will not cause coma even if the corticolimbic reticular activating system or the non-specific projection system of the thalamus in the ipsilateral hemisphere is destroyed. because impulses from the ascending reticular activating system can pass through the other hemisphere to maintain a certain level of arousal. the supratentorial cranial cavity is a non-retractable and almost airtight container that can only be communicated through the canopy. when the space-occupying lesions in the supratentorial cranial cavity gradually increase, the edge of the supratentorial brain tissue will be edematous and displaced, the subarachnoid space will be compressed and occluded, the lateral ventricles will be compressed, and the supratentorial intracranial pressure will increase to the point where supratentorial intracranial pressure becomes incapacitated. when buffering, the supratentorial brain tissue structure is easily displaced downward through the tentorial foramen, forming a subtentorial herniation.
supratentorial space-occupying lesions that cause coma often lead to subtentorial herniation of the cerebellar notch, because as the supratentorial space-occupying lesions gradually increase in size, pressure is conducted downward, and the ascending reticular activating system in the central part of the diencephalon may first pressure or distortion results in inability to awaken, and eventually coma. this is because the center of the diencephalon and the uncus of the temporal lobe are located low and close to the tentorial foramen, which bear greater pressure and are prone to subtentorial herniation. when temporal lobe lesions gradually increase, the uncus of the temporal lobe is most likely to shift infratentorially first, compressing the ascending activation system of the midbrain and causing coma.
tentorial notch hernias can be divided into anterior temporal lobe hernias, posterior temporal lobe hernias, and total temporal lobe hernias. when tentorial notch herniation occurs, brain tissues such as the uncus of the temporal lobe and part of the temporal lobe can shift downward under downward pressure, filling the interpeduncular and circumferential cisterns, thereby compressing the midbrain and oculomotor nerves. the surrounding parasympathetic fibers, etc., lead to pupil dilation, loss of light reflex, and motor element hemiplegia on the contralateral limb on the affected side. if the hernia develops further, it may compress the midbrain and shift to the contralateral side, causing compression of the contralateral cerebral peduncle and corticospinal tract. , causing hemiplegia of the upper motor neurons on the ipsilateral side of the lesion.
when the ascending activation system of the midbrain reticular formation is damaged, varying degrees of consciousness disorders or even coma may occur. if the brain herniation continues to develop and compress the brainstem, the brainstem will be damaged and symptoms such as high muscle tone and decerebral rigidity may occur. the development of cerebral herniation can be demonstrated by the patient's vital signs. in the early stage of brain herniation, due to the early brain herniation compression, the brain stem is ischemic and hypoxic, which excites the brain stem vital center. the patient has deep and rapid breathing, accelerated pulse, and elevated blood pressure. during the compensatory phase of brain herniation, patients may experience slow pulse, deep and fast breathing, and irregular rhythm. mainly due to brainstem compression, ischemia and hypoxia. at this time, the body can still maintain life activities through temporary life center regulation. if cerebral herniation cannot be resolved, or other reasons continue to worsen brainstem ischemia and hypoxia, and brainstem damage gradually worsens, the patient's respiratory and circulatory failure will occur, the central nervous system will be in a state of extreme failure, breathing will become shallow and irregular, and even breathing will stop. , blood pressure drops, arrhythmia, cardiac arrest, and finally death.
Related Information
-
a brief discussion on the mortality rate of hypertensive cerebral hemorrhage
-
how long does it usually take to wake up from coma after brainstem hemorrhage?
-
can patients with cerebral hemorrhage still move their hands when they are in a deep coma?
-
when should i start awakening treatment if i am unconscious due to cerebral hemorrhage?
-
do you have to wake up when you suddenly move in deep coma in patients with cerebral hemorrhage?
-
why does high blood pressure cause coma?